TMD/TMJ Disorders
Temporomandibular Disorders (TMD)
TEMPOROMANDIBULAR DISORDERS (TMD) are a common subgroup of orofacial pain disorders, often incorrectly referred to as "TMJ". TMJ is the commonly used abbreviation for Temporomandibular joint or jaw joint. There are two basic types of TMD: MYOGENOUS TMD (muscle generated pain) and ARTHROGENOUS TMD (jaw joint generated pain.)
TMD SYMPTOMS include pain or discomfort in or around the ear, jaw joint, and/or muscles of the jaw, face, temples and neck on one or both sides. The pain may arise suddenly or progress over months to years with intermittent frequency and intensity. Clicking, popping, grating (crepitus), locking, limited or deviant jaw opening and chewing difficulties are also associated with TMD.
An estimated 75% of the U.S. population have experienced one or more signs or symptoms of TMD. Most TMD symptoms are temporary and fluctuate over time, requiring little or no professional intervention. An estimated 5-10% of the U.S. population will require professional treatment. TMD usually involves more than a single symptom and rarely has a single cause.
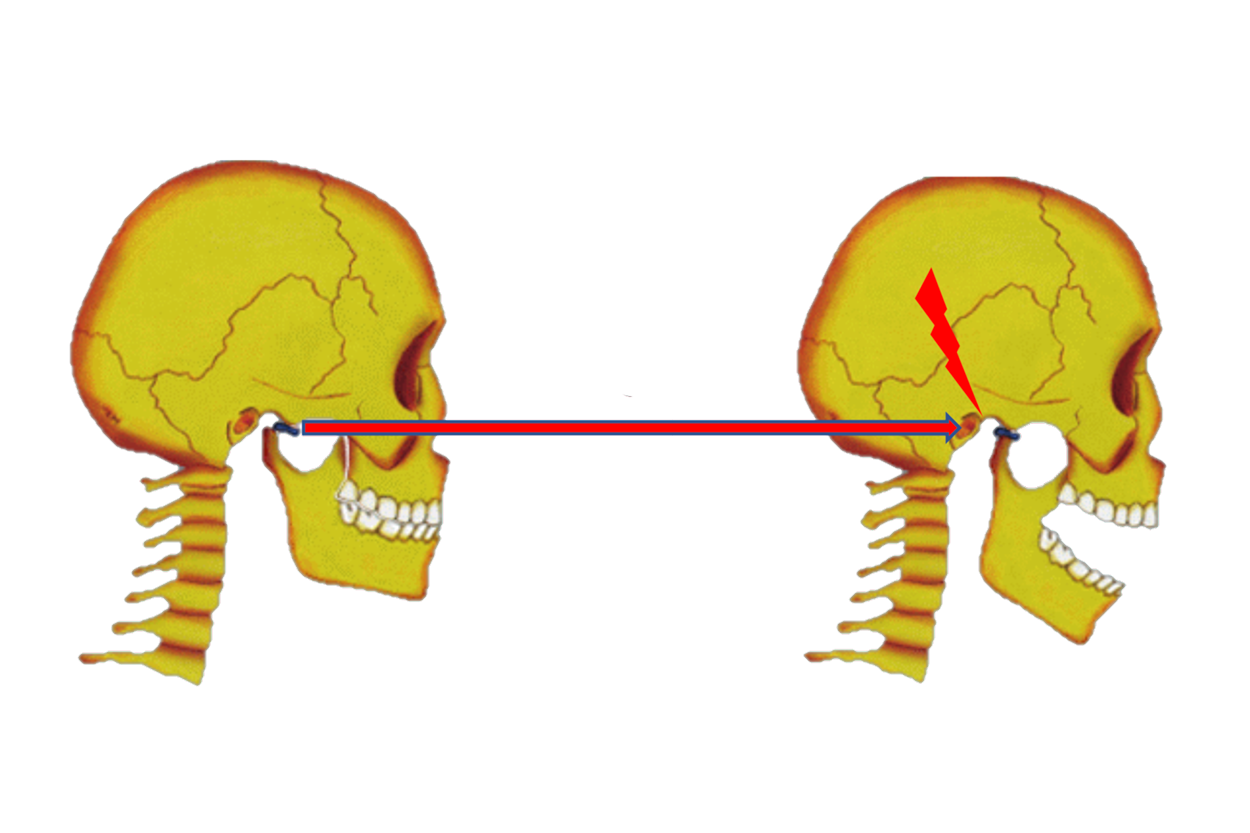
Covid Clench - Recent research studies show people are experiencing increased tooth clenching/grinding and jaw pain since the Covid-19 Pandemic began. If you notice fractured teeth, tooth/jaw/temple pain, clicking/catching/locking or headaches, our team of professionals can help.
TMJ (Jaw Joint) Pain
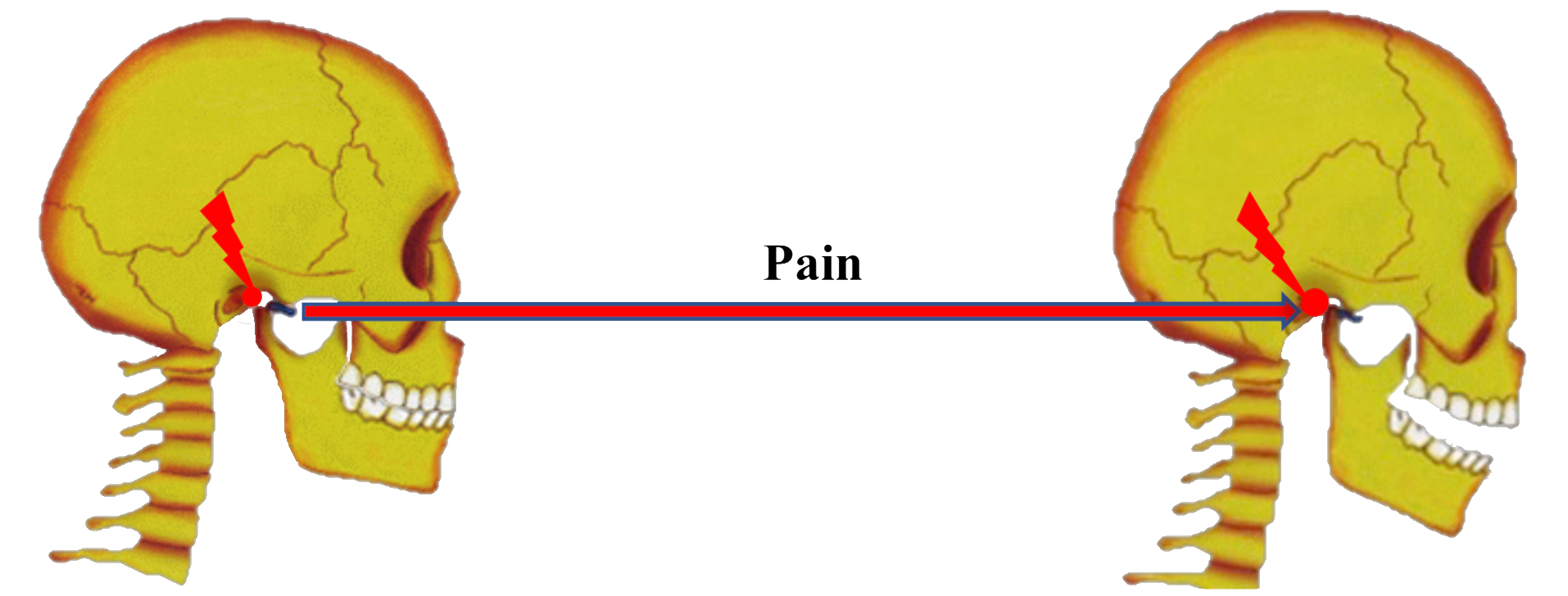
TMJ pain can be caused by an inflammatory process of the synovial lining of the joint. This can be due to infection, cartilage or bone degeneration, trauma or repetitive overuse. TMJ pain is characterized by localized pain over the joint and in front of the ear, that can be aggravated by jaw functional movements such as chewing, yawning and talking, or involuntary dysfunctional movements such as tooth grinding/bruxism and jaw dyskinesia. Jaw Joint pain can also be aggravated and perpetuated by involuntary parafunctional isometric jaw clenching/dystonia. Chronic neck/upper back pain can also increase neck/upper back and jaw muscle tone (clenching), leading to increased TMJ pain. TMJ pain is often referred into the ear, sinus, posterior teeth, temple, behind the eye and down the posterior and lateral neck areas. Swelling inside the TMJ(s) can cause a unilateral or bilateral shift of the jaw when the jaw is fully closed, with subsequent bite changes.
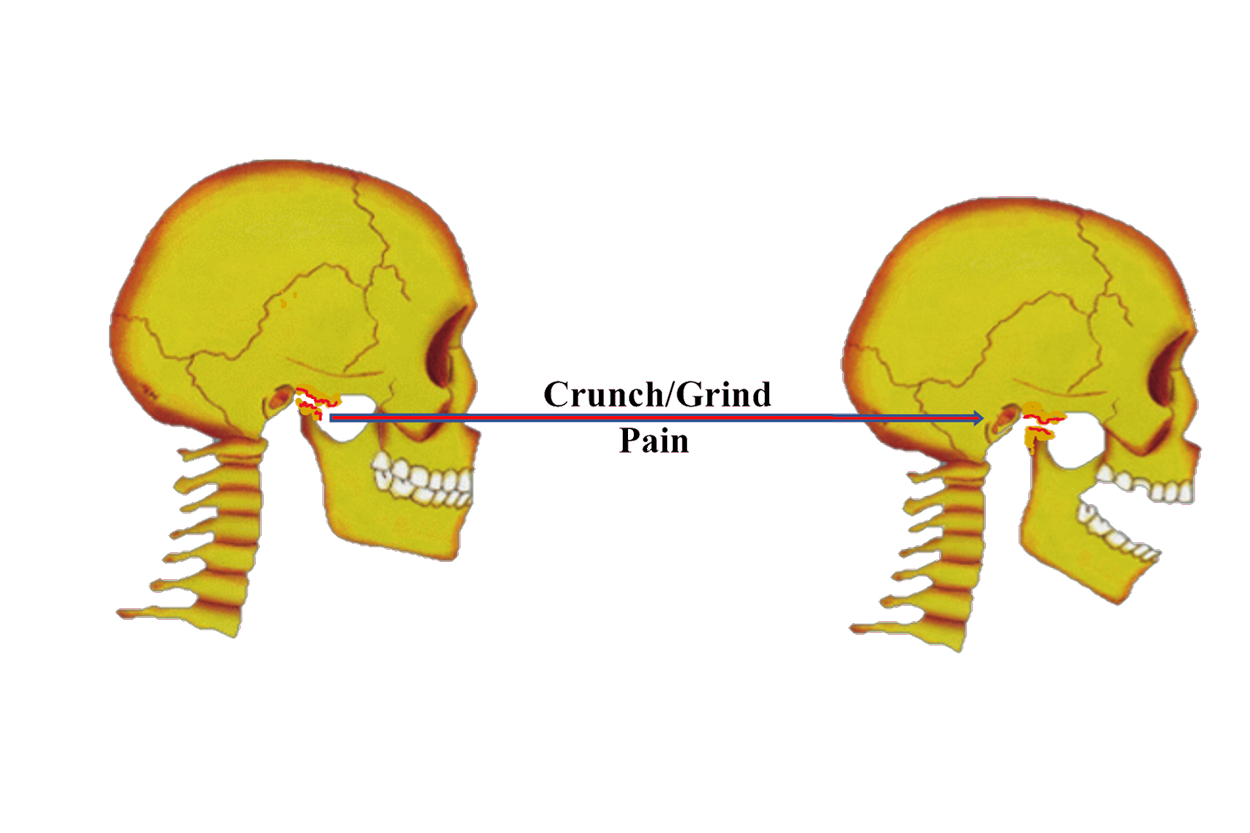
Disc-Condyle Complex Disorders (Jaw Grating/Clicking/Locking):
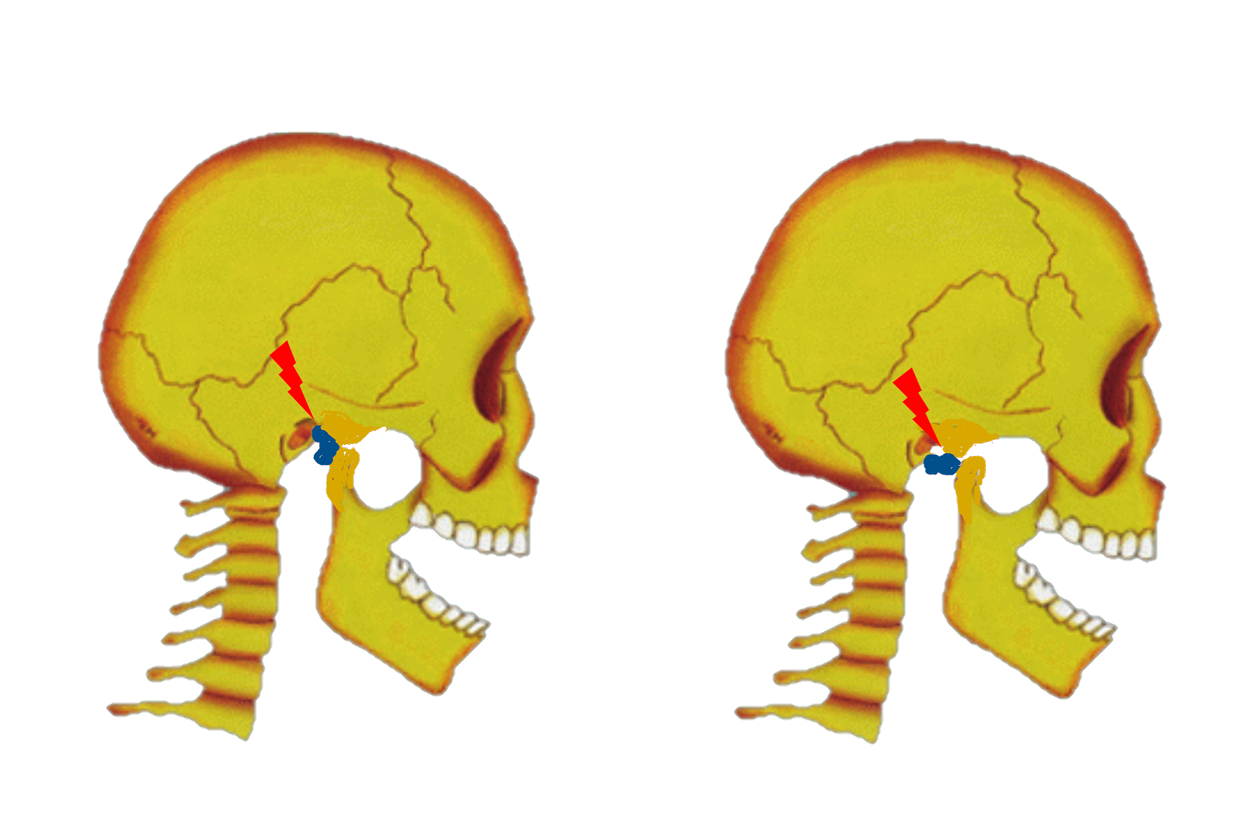
Intracapsular Disc Disorders of the TMJs involve incoordination of the structures that form condyle-disc-ligament complex. When the supportive connective tissue ligaments that stabilize the disc and moving bone structures of the TMJs are sprained/strained (over-stretched) or torn, the collagenous TMJ disc(s) can be displaced/dislocated in abnormal anterior-posterior and/or medial-lateral positions, relative to the condyle, causing grating, clicking, popping or snapping noises as the jaw moves. The lower jaw can lock open or closed if the disc dislocates outside the fossae, blocking the condyle from moving out of (“closed-lock”) or back into the fossa (“open-lock”). Jaw locking/catching can be painful and significantly interfere with the ability to swallow, talk or move the jaw.
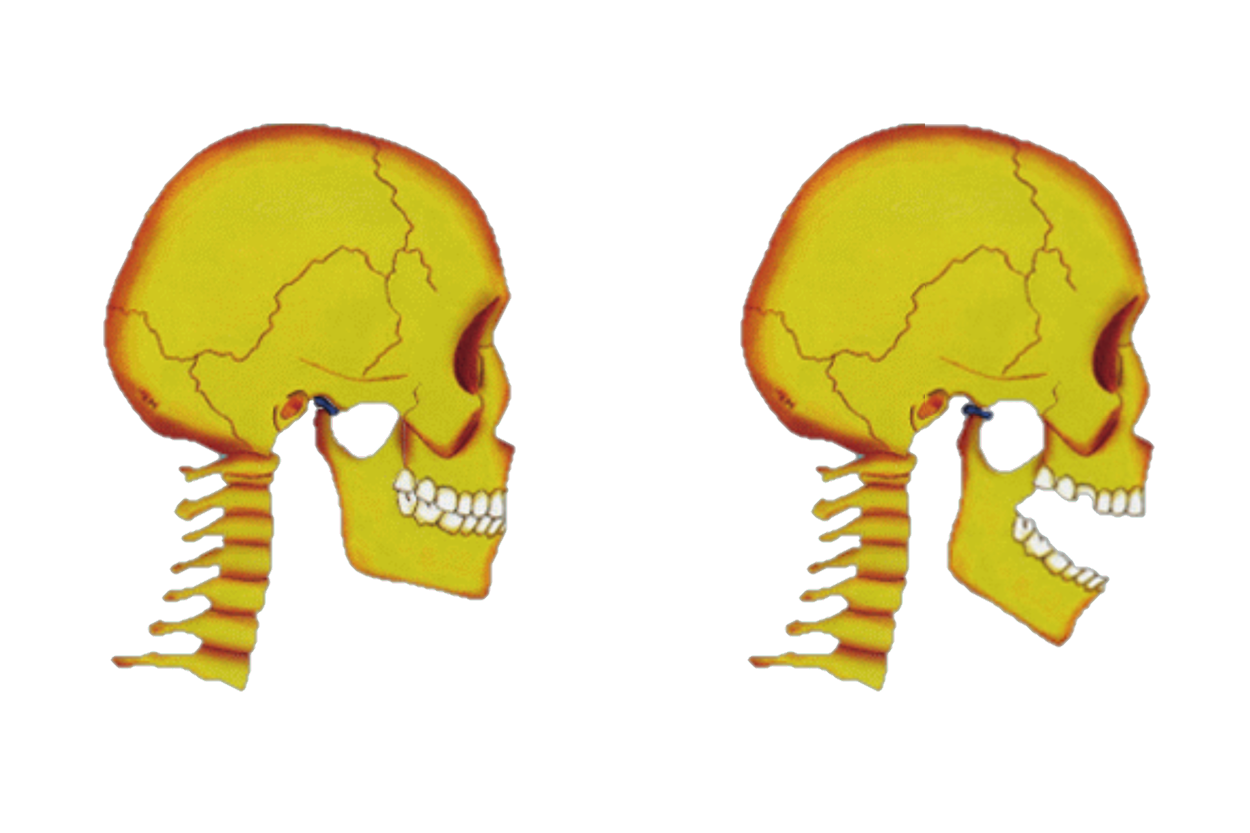
Hypermobility Disorder (Ligamentous Laxity, Anterior Dislocation):
TMJ hypermobility disorders include 2 types of anterior condylar dislocations or “openlock”, related to stretching and/or tearing of the ligaments that stabilize the TMJs during opening and closing. The first type of “open-lock” is called subluxation. Subluxation occurs when the articular disc-condyle complex dislocates outside of the TMJ fossa on opening, anterior to (in-front-of) the articular eminence, and is unable to return back into the TMJ fossa on closing. During subluxation, the TMJ condyle remains in its normal anatomical position on the articular disc, stabilized by the collateral and posterior ligaments, as the entire condyle-disc-ligament complex “subluxates” over the articular eminence on full opening. TMJ subluxation is generally related to excessive laxity or over stretching/tearing of the ligamentous TMJ capsular ligaments that surround and stabilize the joint. The second type of TMJ “open-lock’ is called “luxation”. Luxation occurs when the TMJ condyle translates too far forward, over both the articular eminence and articular disc, on full opening. “Luxation” is related to excessive laxity, tearing overstretching of the TMJ capsular, collateral and posterior ligaments. A specific maneuver or manipulation of the lower jaw may be required, often with local anesthesia and sedation or general anesthesia, to return the “subluxated” articular disc-condyle complex or the “luxated” condyle back into the TMJ fossa to allow the jaw to fully close.